MCW Professor Helps Fellow Native Americans Improve Wellness by Reclaiming Culture
This essay and video were produced by MCW about our Indigenous partners in Lac du Flambeau. The video is narrated by Brian Jackson, EdD, an MCW faculty member and enrolled member of the Ojibwe tribe.
MCW's connection with the community has been featured in previous MedEd Blog posts:
- Take 3 with Brian Jackson, Matt Dellinger and Amy Poupart: Building a Framework to Acknowledge Indigenous Way
- Building Relationships: MCW-Central Wisconsin and the Lac du Flambeau Ojibwe People
- "To be Understood and Appreciated": A Trip to Lac du Flambeau
Released by MCW Communications Office on November 21, 2023
There’s a major phenomenon growing with Indigenous people, according to Brian Jackson, MS, EdD, an assistant professor at the Medical College of Wisconsin (MCW) and member of the Lac Du Flambeau Band of Lake Superior Chippewa Indians, also known as the “Fish Clan.”
“We’re reclaiming our ways,” Dr. Jackson says. “It’s not about asking permission.”
The ways of his people, he says, include harvesting wild rice in autumn, tapping for maple syrup and spearfishing in the spring, and picking medicine throughout the year.
They include sharing foods like deer and fish.
“Elders first,” says Jackson, who added that the practice reinforces ancestral teachings related to taking only what you need and sharing the rest. “They’ll get a package of fish, then the community folks come after that.”
But before they even enter the water for rice, tap the trees or fish or hunt deer, a give and take must take place – an offering of medicine, usually tobacco.
“Those things are really what shaped us,” he says. “We still practice those ways because that’s who we are.”
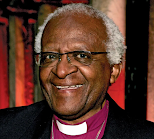
Click on the photo of Dr. Jackson to watch the video:
Unfortunately, some of who they are is also shaped by the historical traumas Native Americans endured during attempts to strip those traditions from them. Among the tragedies, Dr. Jackson says, happened throughout the late 1800s and well into the 1900s, when youths were taken from their families and forced into boarding schools, where their hair was cut and they were forbidden to speak their languages.
“That’s what really halted our language during that time,” he says. “We struggle today to revitalize our language.”
A Feeling of Personal and Native Pride
Dr. Jackson says that reclaiming their languages, traditions and ceremonies are key to improving wellness in Native American communities and overcoming the many challenges it faces, including disparities in cancer and diabetes, and drug and other substance use.
“A lot of folks are struggling with wellness and being sober,” he says. “So we get a person to feel proud again about who they are, and that begins their healing journey pretty well.”
Supporting people on their journeys has been a life mission for Dr. Jackson, who grew up in Milwaukee before moving to the Lac Du Flambeau Reservation in northern Wisconsin as a troubled high schooler.
He credits his grandfather, Joseph Jackson, Sr., who retired after working in the automobile manufacturing industry for 35 years, and father, Dr. Alton Sonny Smart, a professor and Vietnam veteran who speaks fluent Ojibwe, for helping him turn his life around and motivating him to follow the path of education and culture — his two journeys.
Engaging Native Youth
He’s filled many different roles along that journey, including working with youth and families at the Boys and Girls Clubs, with 15-and 16-year-old juveniles at the Woodland Hills Correctional Facility, and with participants of the Family Circle Program in Lac Du Flambeau, and by helping develop the American Indian Science Scholar Program at UW-Milwaukee, which serves students interested in health and science.
“I open their eyes to on-campus experiences, to careers they never even thought of,” says Dr. Jackson, who plans to help develop a similar pathway program for high school students at MCW.
He’s also recently led immersion work that brings non-Native Americans into the reservation for a tour of the community, to meet tribal elders, and experience a powwow at the Indian Bowl.
“It’s about providing opportunities to know our neighbors so we can function and get along,” he shares.
Community-Based Participatory Research
Another major component of Dr. Jackson’s journey has been conducting community-based participatory research as part of the Great Lakes Native American Research Center for Health (GLNARCH) Community Scientific Advisory Committee. Conducting research with Native American communities can be a challenge in a community that is understandably skeptical about being studied.
“How’s it going to benefit our communities?” Dr. Jackson asks. “We’re not just numbers; we want people to be helped.”
Dr. Jackson says a key to research with Native Americans is earning trust and sharing stories.
“You have to sit down with them, take the time, maybe have a meal with them, share some tobacco,” he says. “Not just a one time shot, there’s some follow up to it; that goes a long way with Indian people.”
Dr. Jackson also finds it crucial to collect stories from elders to share with young people as a way of supporting cultural connections.
“We connect them with who they are, their ancestors,” he says. “It’s really the core for anybody for that matter.”
Dr. Jackson views his new role at MCW, which began at the beginning of 2023, as an opportunity to elevate the work he’s done in Indian Country for more than 25 years. It’s also a chance to help more Indigenous communities understand how vital it is to return to traditional values as Native Americans as a way to improve wellness.
“Our values are glossed over at times. It’s about the American Dream,” he says. “The more you get, the more important you are. It’s the opposite with Indian people. If you are sharing and elders see you sharing, that’s what it’s all about.”
Brian Jackson, MS EdD, is an assistant professor in the Department of Epidemiology and Social Sciences at MCW. He serves on the Great Lakes Native American Research Center for Health (GLNARCH) Community Scientific Advisory Committee. He is a Family Circles AODA Prevention Program facilitator, providing instruction in language, traditional cultural practices, history, and culture of Native people will be preserved, thereby restoring pride in the identity of Anishnabe.